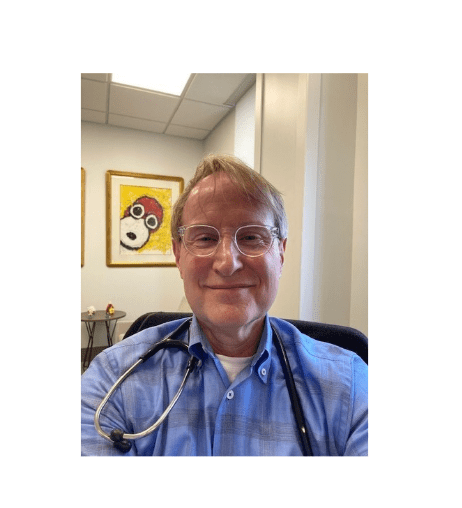
Hear from Dr. Andy Brown, former UMMC medical student, resident, chief resident (x2!) and faculty member. Here, Dr. Brown shares about his time at UMMC, which included 19 years on faculty, and what he’s up to now.
Tell us about you and your time at UMMC.
Let’s see: My dad was a Methodist minister so I grew up all over north Mississippi. I went to Millsaps College – had a blast, made lifelong friends and got a great education. I started medical school in 1985 graduating in 1989. I almost threw up before my first gross exam. I recall one of the older anatomy professors’ nonspecific pointers such as when asked “where is the inferior mesenteric artery?” would make wide arcing waves over the abdominal contents, “it is right there, don’t you see?”. Glad I passed. Being an M3 and M4 was difficult. Back in the day, there were no computers which meant all labs were printed on paper and released at 4 am at a central location in the basement at UMMC. All M3s no matter the service were at the same location, at the same time, fighting for their labs. And, turnaround time was not overnight. As a novice M3, the first task was to learn a new mode of writing: Part Latin, Greek and all abbreviations; once learned it was highly efficient, and kind of cool. Then, how to read and organize a chart. Notes were “SOAP” notes (average 10-15 a day), first written by M3’s, edited by the M4 or intern, then countersigned by the resident and/or an attending. We didn’t have computers or iPhones to look things up as needed. All medical knowledge had to be in your head for rapid recall (e.g. “grilling”) or use your peripheral brain, The Washington Manual, which was always in your coat pocket. An M3 was responsible for all lab draws, starting IV’s, drawing blood cultures, sometimes doing EKGs, etc., i.e. “scut work”. On call M4’s did admissions and ran the floors split with the intern. At the VA, the M4 ran the AO (ED) after hours (YIKES!). Of course, the resident did all admissions, ran the floors, ICU. It was not uncommon to get 15-20 admissions a night at either UMMC or the VA. It was grueling, demanding work. I loved every minute of it.
Now remember, there were no duty hour limits at this time. This was 1989-1990. And, a seismic event occurred my intern year: We did not match a single M4 for the following year’s internship!
The Department was VERY proactive in implementing change. We residents were tasked with providing a list of changes (meetings held with beverages, I think at Leann Fox’s house) needed to improve our work and home quality of life and they were all implemented. A new interim chairman (Pat Lehan, I think), a new resident program director (Mark Meeks, I think), limits to hours worked per week, home by 5 pm post-call, limits to number of admissions per call, limits to number of patients each student responsible per day, MOONLIGHTING AT THE VA (my favorite!), just to name a few. And, it worked – we matched 25 interns the following year!
A downstream effect: I was chief resident two years in a row, a first. During my second chief year, I was also on faculty at the VA. Peggy Miller-Davis and Simon Shikar served as chiefs during their third year of residency. That, too, I believe was a first.
Where are you now?
I live in Atlanta, Georgia. If you threw a dart and hit the center of the city that is where I live: Ansley. And, I work about a mile away at Piedmont Atlanta Hospital. I’m fortunate. I have a very short commute most days. My neighborhood is reminiscent of Belhaven-Bridgewater in Jackson. Sometimes I forget I am surrounded by 7 million people until I try to go to the grocery store and it takes 45 minutes. I had a very large primary care practice but two years ago, Piedmont asked me to start their concierge and executive wellness programs. So, I now have about 500 concierge patients and do executive physicals periodically. I work for Piedmont Healthcare, which has around 3200 physicians who cover 4 million Georgians.
The transition to DIRECT primary care was at first a challenge when I started here in Atlanta. What’s the treatment for strep? Diverticulitis? Anxiety? Patients with multiple conditions and an hour commute to see you, “come back tomorrow” not an option. I’ve worked hard and with time built a pretty solid reputation. Being asked to start a concierge and executive health program for a large healthcare system is something I’m proud of, and I’m proud to say I went to UMMC.
What do you miss about UMMC?
Teaching and the people. I was on faculty for 19 years. During that time, I was fortunate to have taught many students, interns and residents. I hope I had a positive impact on someone and perhaps they recall something I mentioned to them about “how to” in medicine. Lastly, not to dwell on it, but I wish I had told people goodbye. I had a tragedy in my personal life and it was simply too painful to remain in Jackson. Some may not understand; but, it’s fair to say I hope you never do.
Share some memories of your time at UMMC.
- Back in the day, 6W was the medicine ward. It consisted of rooms with 4 to 6 beds and was not air conditioned. This made sweating during rounds even more pronounced, especially since men were supposed to wear ties. I did and taught many blood draws, blood cultures, IVs, lumbar punctures, bone marrows, thoracenteses, etc., on that ward. The nurses were phenomenal and taught a great deal. I learned so much.
- Shirley Schlessinger was my third-year resident when I was an M3. One of her first tasks for me was to disimpact an elderly patient. Within this past year, I have repeated that task twice proving that nothing really changes in medicine.
- John Bowers was my attending with Shirley; we presented cases in the Snavely Library. It was there I learned about Inderal.
- Brent Meadows taught me how to do a thoracentesis my first week as an M3 on medicine. I saw my first CXR with a pneumothorax and a chest tube placed that same day!
- There were only 5 ICU beds at UMMC. Everyone got a central line, art line and a Swan. During my first Swan, I thought the patient was developing an arrhythmia during the procedure – took me a while to figure out the waveforms. Then I realized how awesome it was! I was an M4.
- Jack Reuben of Reuben’s cocktail fame threw an eraser at me when I was an M4 during morning report because I started a patient on antibiotics before getting blood cultures. He was smart but fortunately his aim was poor.
- Ralph Carter and I gave adenosine together for the first time at the VA. We panicked during the brief period of asystole. I think I had it myself.
- Grace Shumaker, Stephanie Elkins and Shirley Schlessinger convinced me to stay in medicine. I was a transitional intern. I was supposed to do anesthesiology.
- Up until my second year of residency, no one slept in the resident dorms. We slept in the resident or student lounges because they were cleaner. Most people didn’t shower post call – the drains didn’t work. I didn’t mind – I wanted to look as tired as I felt. And, yes, I would do it again in a heartbeat.
- LouAnn Woodward was my M3 my intern year at the VA. She used to tell Frank, the resident, and me to stop smoking in, and clean up, the resident office. I have long since stopped smoking but my office is still in disarray (see photo). Got one off my list. But, I can still hear, “Now, Andy,” and “Now, Frank,” and we’d both say, “Yes, ma’am.” We were unsuccessful recruiting her to stay in internal medicine.
- Andre Dadrat, my chief resident, always taught that during a code, take your own pulse first.
- I was paid $12,000 my intern year. Upon reflection, I may have been in poverty, but just didn’t know it. None of us did, I guess.
- I stayed in general medicine because I couldn’t decide on a subspecialty. I liked them all but mostly cardiology and hematology. Now, with time, I would certainly say cardiology.
- My medical training epiphany occurred in September of my intern year. Francesco Simeone was my second year resident. It was my first month as a house intern at UMMC. A heme patient crashed on 5E, Francesco and the M4 were swamped with admissions. I was alone, frightened. I had to sedate, intubate, determine ventilation settings, do central, art line and float a Swan in a matter of a few hours. I promised myself to never have that sense of panic and inadequacy again. Henceforth, my brain became a sponge. I guess everyone must have that moment to find their inner best.
- Doug Harkins mentioned Kodachromes with Dr. Dreiling – some of them were actually on boards. I can still hear him, “Now, here is one for Andy.” Yikes. I’m sweating.
- Griff’s Xrays. Remember Swyer James? Radiation pneumonitis – I can still see that Xray!! “Nature does not create straight lines!” I still recall receiving the phone call when Griff died. I was a pallbearer. He was a good friend and mentor and I miss him.
- Who recalls why Dr. Dreiling suggested a gram stain of the first drop of blood from an earlobe needle prick? I altered antibiotic regimens because of following his advice.
- I first met Michael Hall before I went to medical school when I worked for his father in physiology. I guess he was in middle school. He looks just like his mother. Later, before he went to medical school, Michael worked for me and I proudly wrote him a letter of recommendation. Michael is, and always has been, kind, polite, positive with a brilliant smile and brilliant mind. I was very proud when he was named Chairman.
- I think I was the first, or one of the first, people to teach Mike McMullan how to float a Swan.
- When on call at UMMC, I sometimes took my team down to micro to do sputum and urine gram and AFB stains. Guess the thrown eraser left an impression.
- Doug Harkins listed the greats of the department who taught him: Achord, Lehan, Norman, Thigpen, Turner, etc. I, too, was taught by them. I can see and hear each and every one of them as I am praddling through a diagnostic dilemma. I say that with the greatest respect!
- I did six months of ICU my third year of residency; mostly at the VA.
- Perhaps the best advice: Listen to the patient as they will tell you their diagnosis. Always look the patient in the eyes frequently and touch the patient before you leave the room. I can’t recall who said that to me but I’ve never forgotten it.
- I would do all of it over again if I had to.

How wonderful to hear from Andy. He is absolutely one of the doctors whose example attracted me to internal medicine 30 (yikes!) years ago. I was terrified because I knew I would never know as much as he did, no matter how hard I worked. You are still missed, Andy!
LikeLike
I started out as an intern (1991) prior to an ER residency (I was one of the 24 who matched the year after the IM department matched no one). All the things Andy wrote about were true! I reminisce about those days and certainly learned so much from him! I went on to do radiology (board certified also) but recently became board certified in Obesity Medicine (if anyone knows me, it is a field I am VERY passionate about) and am trying to figure out my place in this world. I often wondered what became of Andy—if you see this would love to reconnect and chat!
LikeLike
Andy was a great guy in college. I haven’t seen him since the college days but I’m sure he is a great doctor.
LikeLike